Pain Management Medical Expert
"Your Path to Pain-Free Legal Solutions"
Case Analysis – Personal Injury – Deposition & Trial Preparation
Table of Contents
Complex Regional Pain Syndrome
Spinal Cord Stimulation
Percutaneous Discectomy
GLP - 1 Receptor Anagonist
Neuropathic Pain
Cervical Radiculopathy
Lumbar Radiculopathy – “Sciatica”
Lumbar radiculopathy, commonly referred to as sciatica, is a condition characterized by pain that radiates along the path of the sciatic nerve, which branches from the lower back through the hips and buttocks and down each leg. This condition typically arises from compression or irritation of the nerve roots in the lumbar spine, often due to factors like herniated discs, spinal stenosis, or bone spurs. Symptoms of lumbar radiculopathy include sharp or shooting pain that may worsen with movement, numbness or tingling in the leg or foot, weakness in the leg muscles, and difficulty walking or standing for extended periods. Lumbar radiculopathy can significantly impact daily activities and quality of life, making it essential to seek medical evaluation and appropriate treatment. Diagnosis usually involves a medical history, physical examination and imaging studies like MRI to confirm the source of nerve compression. Treatment options for lumbar radiculopathy may include medications for pain management and inflammation, physical therapy to improve strength and flexibility, epidural steroid injections or facet joint injections to reduce inflammation around the affected nerve roots, and in severe cases, surgical intervention to relieve pressure on the nerves.

Lumbar Disc Herniation and Extrusion
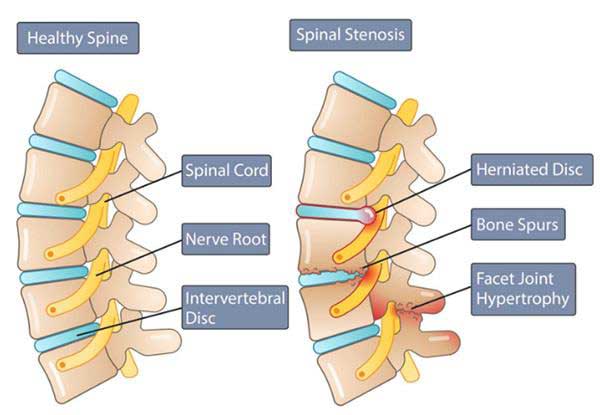
Lumbar disc herniation occurs when the soft cushion-like discs between the vertebrae in the lower back rupture or bulge outwards, putting pressure on nearby nerves. This can result in sharp, shooting pain in the lower back that may radiate down the leg, a condition commonly known as sciatica. Individuals with lumbar disc herniation may also experience numbness, tingling or weakness. Diagnosis typically involves a physical examination and imaging tests like MRI to confirm the location and severity of the herniation. Treatment options for lumbar disc herniation may include rest, physical therapy to strengthen the back muscles, medications for pain management, epidural steroid injections, or in severe cases, surgery to alleviate pressure on the nerves and restore function. Lumbar disc extrusion is a more severe form of disc herniation where the inner core of the disc ruptures through the outer layer and extends into the nerve canal. This condition can cause intense back pain, leg pain, numbness, and muscle weakness. In some cases, lumbar disc extrusion may lead to cauda equina syndrome, a rare but serious condition requiring immediate medical attention due to potential bladder or bowel dysfunction. Treatment for lumbar disc extrusion may involve rest, physical therapy to improve strength and flexibility, medications, epidural steroid injections or surgery.
Lumbar Spondylosis
Lumbar spondylosis, also known as degenerative disc disease and osteoarthritis of the lower back, is a condition characterized by age-related changes in the bones (vertebrae) and discs of the spine. These changes often involve the decrease in height of the discs between the spinal bones, stiffening of the discs, and the growth of bone spurs. While lumbar spondylosis may not always cause symptoms, it is a common cause of spine issues that can range from mild to severe. Symptoms may include back pain and stiffness that worsen in the morning and improve throughout the day, leg pain while standing or walking, numbness, tingling, weakness, or shooting pain. Diagnosing lumbar spondylosis typically involves a thorough evaluation based on symptoms, physical examination, and imaging tests like MRI or CT scans. Treatment for lumbar spondylosis often begins with conservative measures such as ice or heat therapy, over-the-counter pain medications, physiotherapy, and daily exercises to strengthen and stretch back muscles. If these methods are insufficient, more advanced treatments like epidural steroid injections, facet joint injections or surgery may be considered. Management of lumbar spondylosis aims to relieve pain, improve function, and enhance quality of life for individuals affected by this degenerative condition.
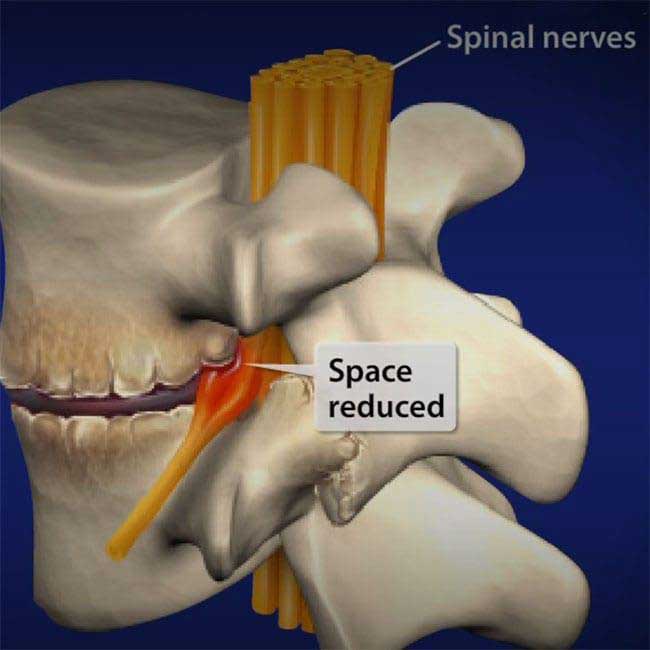
Neuroforaminal Stenosis
Neuroforaminal stenosis, a condition characterized by the narrowing of the openings between vertebrae where spinal nerves exit the spinal cord, can lead to nerve compression and subsequent symptoms. This compression often results in localized back pain that may radiate into the arms or legs, causing numbness, tingling sensations, and muscle weakness. Diagnosis involves a physical examination and imaging studies like as MRI to visualize the extent of nerve compression accurately. Treatment options for neuroforaminal stenosis typically include evaluation by a spine surgeon to decompress the affected nerves, medications for pain relief and inflammation control, physical therapy to enhance strength and flexibility, epidural steroid injections to reduce nerve inflammation, and in severe cases. Managing neuroforaminal stenosis promptly is crucial to alleviate symptoms, improve quality of life, and prevent potential complications associated with nerve compression in the spine. Neuroforaminal stenosis can significantly impact an individual’s daily activities and overall well-being by causing persistent pain and discomfort. Seeking timely medical evaluation for accurate diagnosis is important.
Cervical Spondylosis
Cervical spondylosis, also known as cervical osteoarthritis, is a condition characterized by age-related changes in the bones, discs, and joints of the neck. This degenerative process is primarily associated with the normal wear-and-tear of aging, leading to the gradual breakdown of the cervical spine discs, loss of fluid in the discs, and increased stiffness. As a result of this degeneration, abnormal growths called osteophytes or bone spurs may form on the bones in the neck, potentially causing narrowing of the spinal column or compression of spinal nerves, a condition known as cervical spinal stenosis. Symptoms of cervical spondylosis commonly include neck pain and stiffness, headaches originating from the neck, pain in the shoulders or arms and limited neck movement interfering with daily activities like driving. Diagnosis of cervical spondylosis typically involves a comprehensive assessment that includes a detailed medical history, physical examination focusing on the neck and related areas, reflex testing, strength evaluation in hands and arms, and sensory assessments. Imaging studies like X-rays, CT scans, and MRI scans are often utilized to visualize the structures of the cervical spine for accurate diagnosis. Treatment for cervical spondylosis is usually conservative and may involve rest, nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief and inflammation control, physical therapy including heat and cold therapy or traction exercises, chiropractic manipulation for pain management during severe episodes, wearing a cervical collar for support and limiting movement, and injections like corticosteroids into affected joints or areas surrounding the spine. In rare cases where conservative measures are ineffective or if there is significant spinal cord or nerve compression causing severe symptoms.
Cervical Radiculopathy
Cervical radiculopathy is a condition where a nerve root in the cervical spine (neck region) becomes compressed or irritated, leading to symptoms such as pain, numbness, or weakness that radiate into the shoulder, arm, and sometimes into the hand. This condition is commonly caused by conditions like herniated discs, bone spurs, or degenerative changes in the spine. Symptoms of cervical radiculopathy may include neck pain that radiates into the arm, tingling or numbness in the fingers or hand, weakness in the arm muscles, and difficulty with fine motor skills such as gripping objects or buttoning clothes. Diagnosis of cervical radiculopathy typically involves a combination of physical examination and imaging studies like MRI to pinpoint the location and extent of nerve compression. Treatment options for cervical radiculopathy may include medications for pain relief and inflammation control, physical therapy, epidural injections to reduce inflammation around the affected nerve root, and in some cases, surgery to alleviate pressure on the compressed nerve root. Early intervention and appropriate management can help alleviate symptoms and improve overall function in individuals with cervical radiculopathy.
Complex Regional Pain Syndrome
Complex Regional Pain Syndrome (CRPS) also known as Reflex Sympathetic Dystrophy (RSD) is a chronic pain condition that typically affects one limb following an injury or trauma. This syndrome is characterized by intense pain that may be disproportionate to the initial injury, accompanied by changes in skin color and temperature, swelling, and heightened sensitivity to touch or cold. CRPS is believed to involve abnormal responses in the nervous system and inflammation. Treatment for CRPS often involves a multidisciplinary approach, including physical therapy, medications, nerve blocks, and sometimes psychological support to manage pain and improve function. CRPS can significantly impact daily life and requires prompt medical attention for proper management. Diagnosis of CRPS involves a comprehensive evaluation, including a detailed medical history and physical examination. Treatment options for CRPS include medications for pain relief and inflammation control, physical therapy, sympathetic ganglion blocks, nerve blocks to alleviate pain, and psychological support to address the emotional aspects of chronic pain. Early intervention and treatment are helpful in managing CRPS effectively and improving the quality of life for individuals affected by this condition.
Neuropathic Pain
Neuropathic pain is a complex condition characterized by abnormal hypersensitivity to stimuli, often described as shooting or burning pain. It can be chronic, unrelenting, and severe, resulting from nerve damage or a malfunctioning nervous system. Causes of neuropathic pain include various conditions like diabetes, chemotherapy, spinal cord compression, and infections like HIV or shingles. Symptoms may manifest as shooting and burning pain, tingling, and numbness. Diagnosing neuropathic pain involves an evaluation by a physician, including interviews, physical exams, and nerve tests. Neuropathic medication, such as anticonvulsant and antidepressant drugs, are commonly used as first-line treatments, with non-steroidal anti-inflammatory drugs (NSAIDs) like Aleve or Motrin sometimes easing pain. In cases where the pain is challenging to manage, a pain specialist may recommend invasive or implantable devices like a spinal cord stimulator. Other treatment options include physical therapy, counseling, relaxation therapy, massage therapy, and acupuncture.
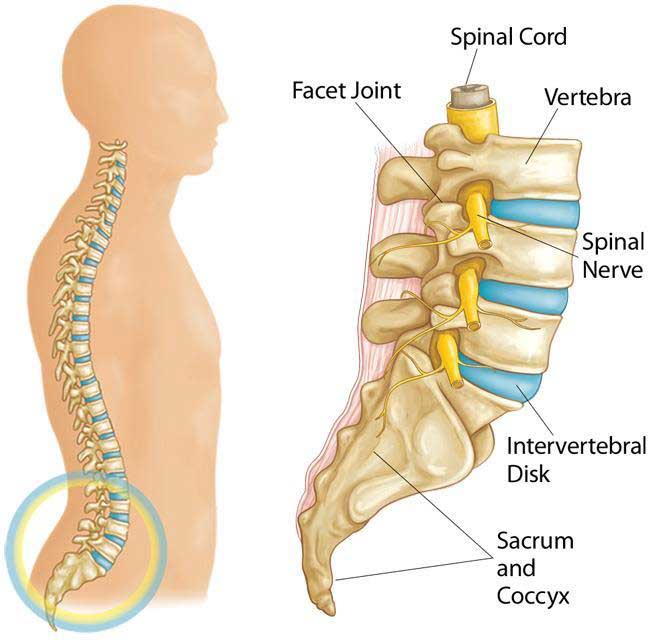
Lumbar Spinal Stenosis
Lumbar spinal stenosis is a condition characterized by the narrowing of the spinal canal in the lower back, leading to pressure on the spinal cord and nerves. This is a common condition found in the elderly population. This narrowing can result from various factors, including degenerative changes associated with aging, such as arthritis and degeneration of the intervertebral discs. Symptoms of lumbar spinal stenosis often include low back pain, radiating pain into the buttocks and legs, numbness, tingling sensations, muscle weakness, and difficulty walking long distances. Diagnosis typically involves a comprehensive evaluation by a healthcare provider, including a physical examination and imaging tests like X- rays, CT scans, or MRI scans. Non-surgical options like physical therapy, medications for pain relief and inflammation control, and steroid injections are often considered first. In cases where conservative measures are ineffective, surgical interventions like laminectomy or spinal fusion may be recommended to alleviate symptoms and create more space within the spine.
Diabetic Neuropathy
Diabetic neuropathy is a type of nerve damage that can occur in individuals with diabetes due to high blood sugar levels that can injure nerves throughout the body. This condition most commonly affects nerves in the hands and feet, leading to symptoms like pain, numbness, and tingling sensations in these areas. Depending on the type of diabetic neuropathy, individuals may also experience issues with the organs of the body. There are many different types of diabetic neuropathy and each type presents with distinct symptoms affecting different parts of the body. Prompt medical attention is crucial if individuals experience symptoms like burning, tingling, weakness, or pain in their hands or feet that interfere with daily activities or sleep. Preventing diabetic neuropathy or slowing its progression is achievable through consistent blood sugar management and a healthy lifestyle. Individuals with diabetes are advised to maintain their blood sugar levels within target ranges to reduce the risk of nerve damage.
Shingles
Shingles, caused by the varicella-zoster virus, is a viral infection that can lead to a painful rash. This condition typically occurs in individuals who have previously had chickenpox, as the virus remains dormant in the body and can reactivate later in life. The rash associated with shingles often appears in a band-like pattern on one side of the body and progresses into fluid-filled blisters. Alongside the rash, individuals may experience symptoms such as burning, sharp, or jabbing pain in the affected area, which can persist even after the rash has healed. Factors like age, severity of the shingles episode, presence of other medical conditions like diabetes, location of the shingles outbreak, and delay in seeking treatment can increase the risk of developing complications such as post-herpetic neuralgia (PHN). Vaccines like Shingrix are recommended for adults to prevent shingles and reduce the likelihood of complications. Shingles can be a painful and uncomfortable condition that significantly impacts an individual’s quality of life. Education about shingles symptoms, risk factors, and preventive measures such as vaccination is essential for raising awareness and promoting proactive healthcare practices to minimize the impact of this viral infection.
Post-Herpetic Neuralgia (PHN)
Post-herpetic neuralgia (PHN) is a common complication of shingles characterized by persistent nerve pain that continues after the shingles rash has healed. This condition can cause long-term discomfort, with symptoms including burning, sharp, jabbing pain in the area where the shingles rash occurred, sensitivity to touch, itching, or numbness. Risk factors for developing PHN include advanced age (typically older than 60), severity of the initial shingles episode, presence of underlying medical conditions like diabetes, location of the shingles outbreak on the body, and delays in receiving antiviral treatment. Preventative measures such as vaccination against shingles are recommended to reduce the risk of developing PHN and other complications associated with shingles infections. Managing post-herpetic neuralgia involves a multidisciplinary approach aimed at alleviating pain and improving quality of life for individuals affected by this condition. Treatment options may include medications for pain relief such as anticonvulsants or antidepressants, topical treatments like lidocaine patches, nerve blocks to target specific areas of pain, physical therapy, and complementary therapies like acupuncture or relaxation techniques.
