Pain Management Medical Expert
"Your Path to Pain-Free Legal Solutions"
Case Analysis – Personal Injury – Deposition & Trial Preparation
Table of Contents
Complex Regional Pain Syndrome
Spinal Cord Stimulation
Lumbar Disc Herniation and Disc Extrusion
Percutaneous Discectomy
GLP - 1 Receptor Antagonist
Neuropathic Pain
Cervical Radiculopathy
Spinal Cord Stimulation
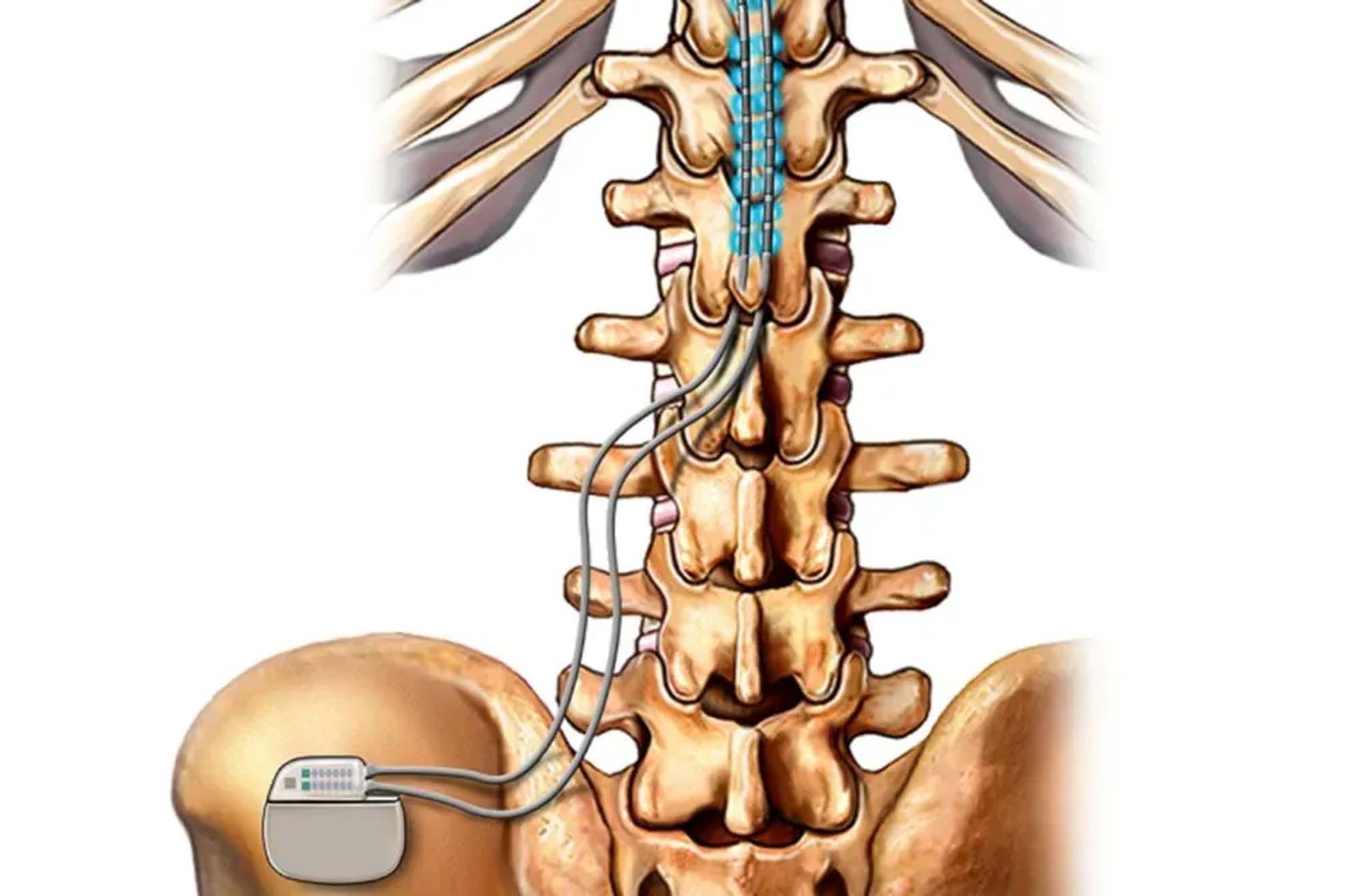
Spinal cord stimulation (SCS) is a pain management technique involving the implantation of a device that emits electrical impulses to the spinal cord. These impulses modify pain signals before they reach the brain, often replacing them with a non-painful tingling sensation called paresthesia. The procedure typically begins with a trial phase, where temporary leads are placed in the epidural space near the spinal cord under local anesthesia. The leads are connected to an external pulse generator worn by the patient. Over the course of a week, the patient evaluates the effectiveness of the therapy. If significant pain relief is achieved, a pain management physician then performs the permanent implantation of the system, which includes placing permanent leads and an implantable pulse generator (IPG) under the skin, usually in the abdomen or buttocks.
Common Diagnosis
Common diagnoses treated with spinal cord stimulation include post-laminectomy syndrome, complex regional pain syndrome (CRPS) and peripheral neuropathy. Post-laminectomy syndrome involves persistent pain following spinal surgery, while CRPS is a chronic pain condition usually affecting the limbs. Peripheral neuropathy refers to nerve damage outside the brain and spinal cord, often resulting in pain, tingling, and numbness. SCS can significantly improve the quality of life for patients with these chronic pain conditions by reducing their pain perception and reliance on pain medications.
Percutaneous Discectomy
Percutaneous discectomy is a minimally invasive procedure used to remove a portion of a herniated disc that is pressing on a nerve root or the spinal cord. This technique involves inserting a needle through the skin and into the disc under imaging guidance, such as fluoroscopy. A pain management physician typically performs this procedure by first administering local anesthesia to the area and then using specialized tools, often through the needle, to extract the herniated disc material. The goal is to relieve pressure on the nerves and reduce pain, numbness, and other symptoms associated with disc herniation.
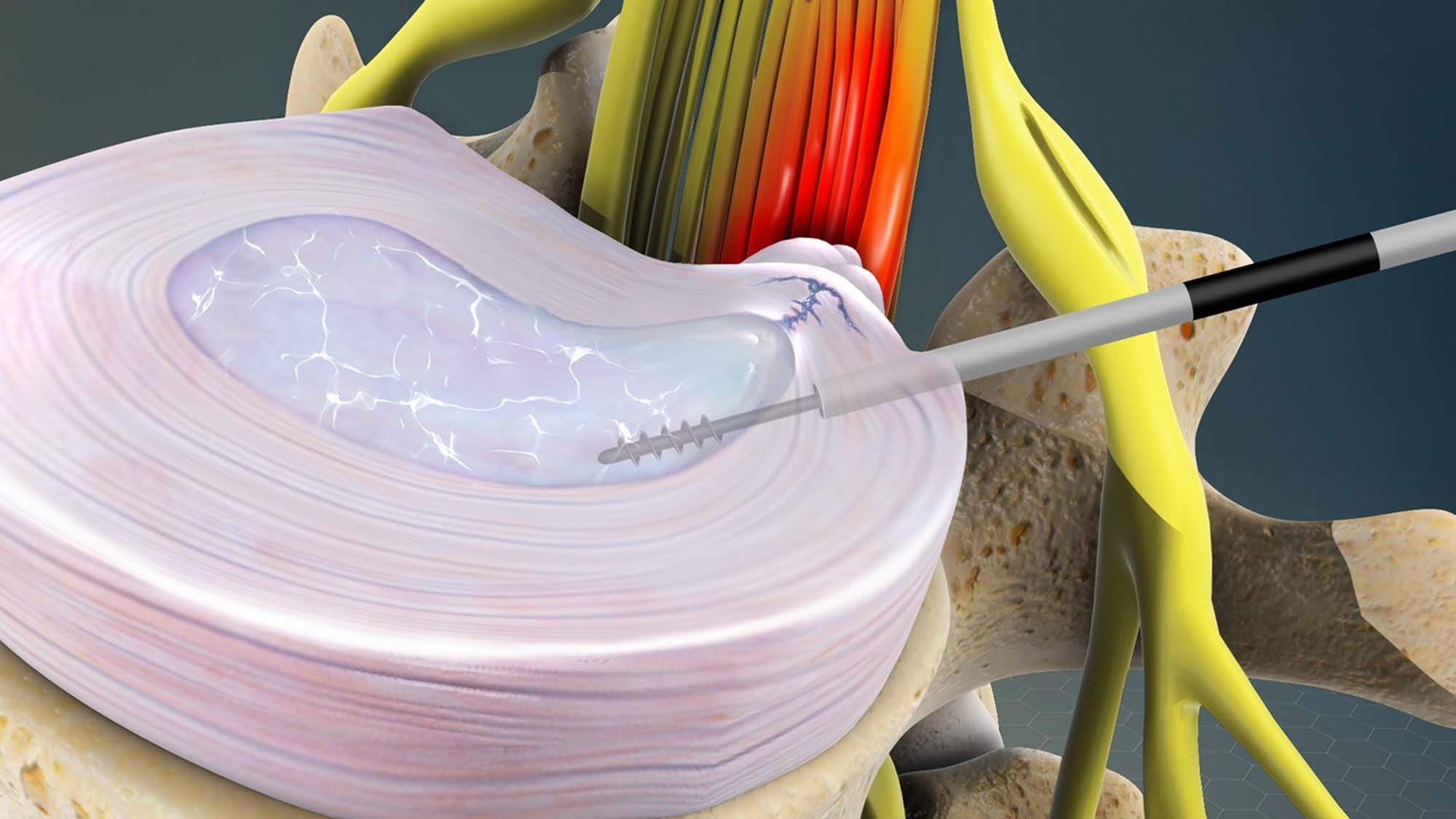

This procedure is commonly indicated for patients with specific diagnoses, including herniated discs, bulging discs, and contained disc herniations that cause radicular pain, often referred to as sciatica when affecting the lower back and legs. Patients who have not responded well to conservative treatments such as physical therapy, medications, or epidural steroid injections may benefit from percutaneous discectomy. It is particularly useful for those experiencing significant nerve compression symptoms without extensive disc degeneration or spinal instability, providing pain relief and improving function with a less invasive approach compared to traditional open surgery.
